Depression and Comorbidity with Cardiometabolic Disorders
Background
Major depressive disorder (MDD) and cardiovascular disease (CVD) are the two primary causes of disability worldwide. Women are at twice the risk for MDD and heart disease is the primary cause of death for women and men. Co-occurrence of MDD and CVD was slated to be #1 cause of disability worldwide in 2020 and women are at twice the risk, leading to a 3-5-fold risk of death in women from heart disease, often with unrecognized and untreated MDD.
MDD is associated with abnormalities in stress response circuitry which contain highly sexually polymorphic brain regions. We and others demonstrated that activity in these areas was associated with steroid hormone, immune, autonomic, and vascular responses, which differed by sex.
Understanding early biomarkers for sex differences in this comorbidity will provide knowledge for early intervention, attenuating and potentially preventing disorder and disability later in life.
Our Work
Our team investigates fetal and neonatal programming of sex differences in the healthy brain and expression of sex differences in adulthood. We examine hormonal, immune, and genetic regulation of brain morphology/function using multi-modal MRI/DTI technologies and associated physiology. We use a lifespan approach, given that we have followed a unique prenatal cohort over the last 30 years who are now (in 2022) aging into their 60’s.
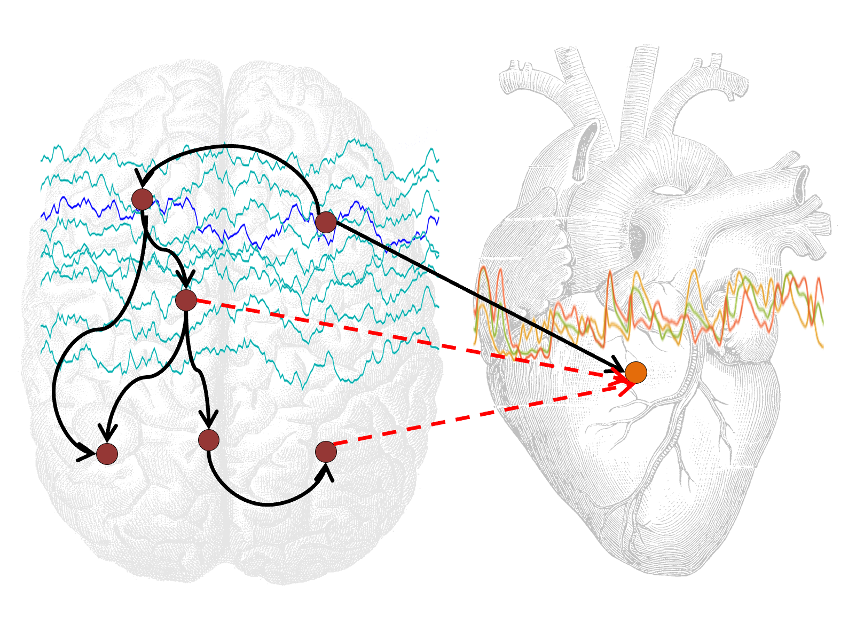
We use multimodal imaging approaches (e.g., sMRI/fMRI/DTI) acquired during in-scanner stress tasks coupled with hormone, immune, ANS and other cardiac functions, and relate brain and physiology outcomes to early developmental exposures and biomarkers for identifying sex differences in risk for comorbidity of depression and CVD. Further, genetic/genomic/ transcriptomic approaches are used to identify genetic pathways of interest.
U54 SCORE NIH ORWH Grant (2020-2025)
In 2020, the NIH Office for Research on Women’s Health and National Institute of Mental Health jointly supported 5-year $8.3 million SCORE grant.
Through three synergistic basic science and clinical translational studies, we are investigating the early developmental origins of sex differences in the comorbidity of depression with cardiac and neurovascular dysfunction.
Further, we are leveraging the discoveries into development of a novel neuromodulation therapeutic device targeted to the neural-cardiac interface.
Finally, we are training the next generation of scientists to enhance discovery of sex differences in the brain and the vasculature to develop novel therapies.
For more information visit the SCORE Website
A Sample of Key Findings
One.
fMRI results showed that exposure to pro-inflammatory cytokines in utero was significantly associated with sex differences in brain activity and connectivity during response to negative stressful stimuli 45 years later
Two.
Fetal risks (i.e., fetal growth restriction/preeclampsia) were significantly associated with loss of cardiac tone (low high frequency heart rate variability (HF-RRV), which was 3 x stronger in people with major depression. Females had a higher risk of comorbidity of MDD and low HF-RRV than males
Three.
Depression and loss of cardiac function comorbidity shared brain circuitry regulating response to negative stress in a sex-dependent manner
Four.
Mechanisms implicated in sex differences in risk for comorbidity include steroid hormone, immune, metabolic, and vascular pathways
Highlighted Works.
Impact of sex and depressed mood on the central regulation of cardiac autonomic function